Working group Clinical Neurochemistry (AG Tumani)
Research focus and aims:
The main focus of the Clinical Neurochemistry working group is the understanding of the pathological processes that underly neuroinflammatory and neurodegenerative disorders, as well as their (early) diagnosis and monitoring using fluid biomarkers. For that purpose, we identify and evaluate biomarker candidates and establish novel biomarker assays for the detection of proteins in cerebrospinal fluid (CSF) and blood, applying highly sensitive state-of-the-art immunoassay methods e.g., single-molecule array (Simoa) or microfluidic systems (ELLA). We aim to thoroughly evaluate and validate potential new biomarker assays, both regarding their relevance as diagnostic, prognostic, or progression markers in inflammatory and neurodegenerative diseases, as well as regarding the applicability and validity of the assay itself for the use in clinical routine. In addition to assay development, we conduct single- and multicenter studies using existing or novel biomarker assays. These studies aim to investigate correlations between biomarkers and clinical evaluations to learn more about how these markers could be effectively implemented into daily clinical practice. As a translational working group our ultimate objective is to successfully transfer these biomarkers into clinical routine, allowing patients to benefit from improved diagnostic accuracy and enabling personalized patient care.
Group members Clinical Neurochemistry

Prof. Dr. med. Hayrettin Tumani
Senior Consultant Neurologist
Head of Laboratory for CSF Diagnostics and Clinical Neurochemistry
Head of Outpatient Unit MS and neuroinflammatory Diseases
*Kontakt
E-Mail: hayrettin.tumani@uni-ulm.de
Telefon: +49 731 500 63010
Fax: +49 731 500 63002
Anschrift:
Klinik und Poliklinik für Neurologie der Universität Ulm
Oberer Eselsberg 45
D-89081 Ulm
Link to CSF diagnostic lab: https://www.uniklinik-ulm.de/neurologie/laboratorien/liquorlabor.html
Link to MS study group: https://www.uniklinik-ulm.de/neurologie/sprechstunden-ambulanzen/multiple-sklerose-und-entzuendliche-zns-erkrankungen.html

Dr. rer. nat. Steffen Halbgebauer
Junior Group Leader AG Translational Biomarker Development
*Kontakt
E-Mail: steffen.halbgebauer@uni-ulm.de
Telefon: +49 731 500 63112
Fax: +49 731 500 12 63112
Anschrift:
Zentrum für Biomedizinische Forschung (ZBMF)
Helmholtzstr. 8/1
D-89081 Ulm
Link zur Juniorarbeitsgruppe „Translational Biomarker Development“

Martina Hospes
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 500 63010
Fax.: +49 731 500 63002
Mail: martina.hospes@uniklinik-ulm.de

Dr. rer. nat Franziska Bachhuber
M.Sc. Molecular Medicine
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 177 5525
Fax.: +49 731 177-1592
Mail: franziska.bachhuber@uni-ulm.de

Dr. rer. nat. André Huss
M.Sc. Biology
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Mail: andre.huss@uni-ulm.de

Dr. med. Deborah Erhart
Neurologist
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 177 5381
Mail: deborah.erhart@uni-ulm.de

Luisa Balz
Neuropsychologist
M.Sc. Psychology
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Mail: luisa.balz@rku.de


Jonas Schaller
Resident of Neurology
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Mail: jonas.schaller@uni-ulm.de

Paula Klassen
M.Sc. Molecular and Translational Neuroscience
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 177 5375
Mail: paula.klassen@uni-ulm.de

Badrieh Fazeli
M.Sc. Biology
Anschrift:
Zentrum für Biomedizinische Forschung (ZBMF)
Helmholtzstr. 8/1
D-89081 Ulm
Tel.: +49 731 500 63010
Mail: badrieh.fazeli@uni-ulm.de

Christoforos Alexudis
Human Medicine
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm

Lukas Gmelch
MD, Human Medicine
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm

Stephanie Sckell
MD, Human Medicine
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm

Tatjana Simak
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 177 1519
Fax.: +49 731 177 1592

Dagmar Schattauer
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 177 5254
Fax.: +49 731 177 1592″
Mail: neurobiobank@uni-ulm.de

Sandra Hübsch
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 177 5254
Fax.: +49 731 177 1592
Mail: neurobiobank@uni-ulm.de

Alice Beer
Anschrift:
Oberer Eselsberg 45
D-89081 Ulm
Tel.: +49 731 177 5254
Fax.: +49 731 177 1592
Mail: neurobiobank@uni-ulm.de
Research interests / Disease groups:
The neurological diseases our research focuses on can generally be stratified into two primary groups: neuroinflammatory and neurodegenerative diseases. Among the group of inflammatory diseases of the central nervous system our primary focus lies on multiple sclerosis (MS) and related autoimmune and demyelinating diseases such as neuromyelitis optica spectrum disorders (NMOSD) and MOG antibody-associated diseases (MOG-AD). We are particularly interested in the identification and evaluation of candidate biomarkers to assess disease activity, predict progression, and monitor treatment effects. For the neurodegenerative group we aim to improve the (early) diagnosis and the readout of the efficacy of therapeutic agents in clinical trials for Alzheimer’s disease (AD), amyotrophic lateral sclerosis (ALS) and Parkinson’s disease (PD).
In addition to our primary focus on biomarker candidate identification, assay development, validation, and clinical translation of new developments for the analysis of CSF and blood samples, we are also interested in exploring novel biological materials and research fields, such as investigating tear fluid or conducting microbiome analysis. More recently we have expanded our research focus to the investigation of Long-COVID syndrome with the aim to integrate clinical, radiological, neuropsychological, and neurochemical parameters in the research.
A focus on patient-oriented research and a strong connection between research and clinical practice are of major importance to us. We benefit significantly from our multidisciplinary team and our close collaboration with the clinical MS study group and the routine CSF diagnostic laboratory.
Applying biomarkers as objective readout measures in clinical trials or to improve early (differential) diagnosis and enable prediction of disease progression is a major research focus of our working group. For that reason, we have a special interest in brain-derived markers that represent specific pathological processes in the central nervous system. One such marker, indicating axonal damage are neurofilaments. We already incorporated neurofilament proteins into our routine analysis for the differential diagnosis of ALS (more information can be found in the section “Routine analysis” and on the homepage of our CSF laboratory
(https://www.uniklinik-ulm.de/neurologie/laboratorien/liquorlabor.html).
However, as there are still open questions regarding the use of neurofilament analysis in other neurological diseases, we investigate their potential as biomarkers for prognosis or disease monitoring. Another marker we are interested in, representing astrocytic damage, is the Glial acidic fibrillary protein (GFAP). GFAP is found to be elevated e.g., in blood of AD patients and seems to be a disease progression marker in MS. Furthermore, we also work on synaptic proteins such as beta-synuclein or SNAP-25 which could enable an early diagnosis of neurological diseases as synaptic deterioration occurs early in the disease course of many neurological diseases.
In the Neuro-Biobank with a focus on neurodegenerative (ALS, dementia, Parkinson's) and inflammatory (multiple sclerosis, neuroborreliosis, acute meningoencephalitis) diseases biological samples are preserved with the approval of the ethics committee and the patients’ consent. The standardized biobanking mainly focuses on CSF, serum, and plasma samples and is extended to other biomaterials such as urine, tears, skin, and DNA in the context of specific research questions. The samples are utilized to assess the clinical relevance of new diagnostic tests, in biomarker projects, as well as in scientific collaborations.
We work in close collaboration and proximity to the routine laboratory for CSF diagnostics. The laboratory for CSF diagnostics and clinical neurochemistry is one of the training laboratories certified by the German Society for CSF diagnostics and clinical neurochemistry (DGLN) and is accredited by the German Accreditation Body (DAkkS). Patient samples from the in- and outpatient units of the department of Neurology of the University Hospital Ulm as well as from external senders are analyzed. The laboratory for CSF diagnostics offers a broad spectrum of parameters, covering all methods of routine CSF analysis as outlined in the S1 guidelines on lumbar puncture and cerebrospinal fluid analysis (https://doi.org/10.1186/s42466-020-0051-z) as well as an extensive spectrum of special parameters. New developments that were integrated into the spectrum of methods in the recent years include dementia markers (pTau, amyloid-beta ratio) for degenerative CNS diseases, CXCL13 and free (kappa/lambda) immunoglobulin light chains for inflammatory CNS diseases, as well as autoimmune-antibody diagnostics for paraneoplastic syndromes, autoimmune encephalitis, and NMOSD/MOG-AD. For more information on the currently offered parameters of CSF analysis please visit the homepage of the CSF laboratory (https://www.uniklinik-ulm.de/neurologie/laboratorien/liquorlabor.html).
In addition to routine services, we also analyze the neurofilament light (NfL) chains in serum and phosphorylated neurofilament heavy (pNfH) chains in CSF on a weekly basis in our routine laboratory. Hereby we established cut-offs for the differential diagnosis of ALS. More information and the requisition slip can be found on the homepage from our CSF laboratory (https://www.uniklinik-ulm.de/neurologie/laboratorien/liquorlabor.html).
We belong to national and international networks of specialized centers and are involved in the collection of biomaterials to build up large bio-depositories to enable research focused on the spectrum of neurodegenerative diseases which are often very rare.
Our group initiated the German Research Consortium of frontotemporal lobar degeneration to develop and evaluate parameters which help clinicians to diagnose FTLD at an early stage and follow its progression, with the overall aim to develop effective objective targets for therapeutic strategies (www.ftld.de). As this was successful, we have now started clinical trials in FTLD, investigating an active immunotherapy directed against pathologically modified tau protein that is the main constituent of pathological changes in nonfluent variant of PPA.
An important point for the implementation of fluid biomarkers into clinical routine is the standardization of sample collection, processing and storage. We are involved in several international networks with the aim to advance standardization in CSF analysis (BiomarkAPD, SOPHIA, CSF Society, KKNMS) and regularly provide workshops on basic knowledge to work with CSF.
- Enzyme-linkend immunosorbent assay (ELISA)
- Single molecule array (Simoa)
- Capillary isoelectric focusing for PTM analysis (NanoPro 1000)
- Microfluidic ELLA technology
- Real-Time Quaking-Induced (RT-QuIC) conversion assay
- Nanoparticle tracking analysis (NanoSight)
- Lumipulse G600II (automated assays for core AD biomarkers)
- Western Blots
- Isoelectric focusing for the identification of oligoclonal IgG bands in CSF and serum (OCB)
- CSF analysis (e.g., basic and special parameters, evaluation by quotient diagrams, Reibergrams, pathogen-specific antibody indices)
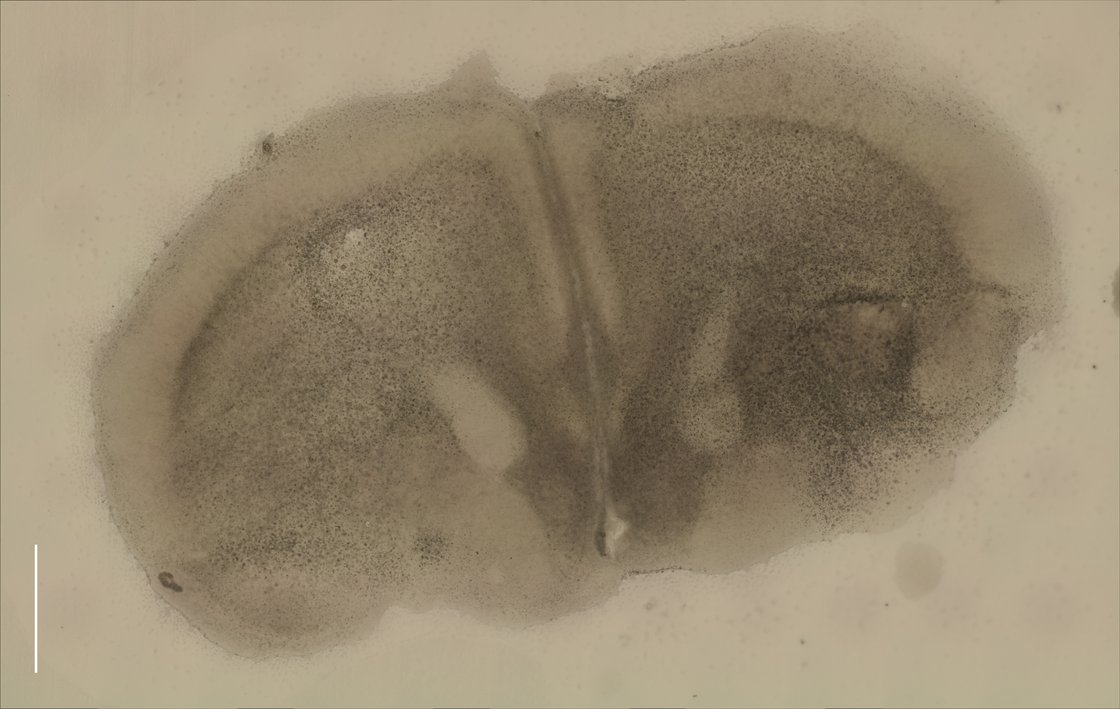
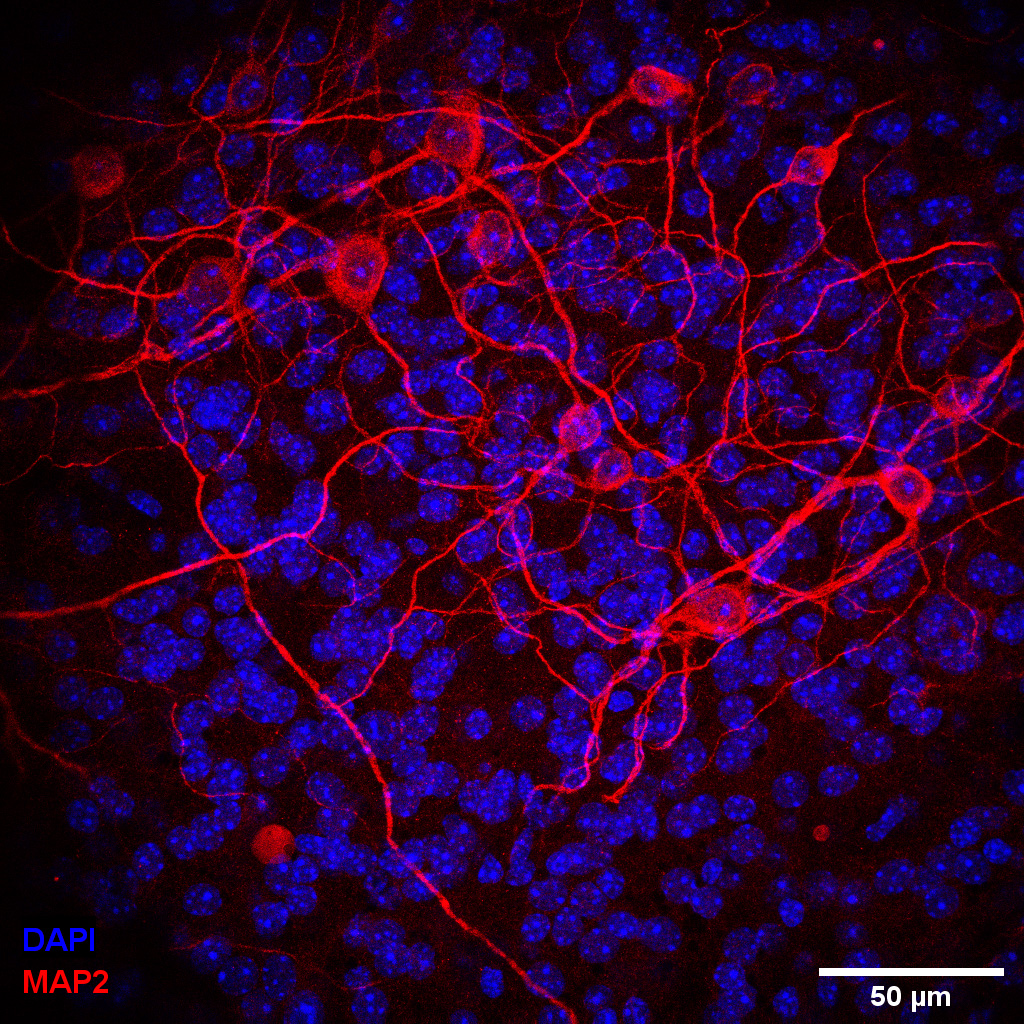
- Organotypic brain slice culture
- Immunohistochemistry
Cooperations & Partners
Motor Neuron Disease / Motor System Disorders Outpatients
Head: Prof. Dr. A. C. Ludolph, Prof. Dr. J. Dorst, Dr. R. Gastl
Amyotrophic Lateral Sclerosis / Models of Motor System Disorders
Head: Prof. Dr. med. A.C. Ludolph, Prof. Dr. F. Roselli
Neuroproteomics and Biomarker Research
Head: PD Dr. biol. hum. Patrick Öckl
Molecular and Translational Neuroscience; MTN
Head: Prof. Dr. rer. nat. L. Dimou
Clinical Neuroanatomy: Anatomy and Pathology of Cerebrovascular Disorders
Head: Prof. Dr. D. Yilmazer-Hanke
Molecular mechanisms of neurodegeneration
Group management: Prof. Dr. K. Danzer
Translational protein biochemistry (DZNE),
Institute of Anatomy and Cell Biology
Head: Prof. Dr. Tobias M. Böckers
Systemic neurosciences, systemic neuroscience laboratory
Head: Prof. Dr. F. Roselli
Dementia Diseases: Clinical care
Head: PD Dr. Sarah Jesse
Neuropsychology
Head: Prof. Dr. I. Uttner, Prof. Dr. D. Lulé
CSF Laboratory – Autoimmune Laboratory
Prof. Dr. Hayrettin Tumani, PD Dr. Sarah Jesse, Prof. Dr. J. Lewerenz
Neuroinflammatory Diseases, Subspecialty Multiple Sclerosis
Head: PD Dr. M. Senel, Prof. Dr. H. Tumani
Prof. Dr. Markus Otto
Department of Neurology,
Martin-Luther-University Halle-Wittenberg
Ernst-Grube-Straße 40
01620 Halle-Saale
Germany
Prof. Dr. Lucilla Parnetti
Department of Medicine and Surgery
University of Perugia
Italy
Dr. Ahmed Abdelhak, MD
School of Medicine
675 Nelson Rising Lane, #260
San Francisco CA 94158
- DGLN – German Society for CSF Diagnostics and Clinical Neurochemistry - http://www.dgln.de/
- CSF Society – European Society for CSF Analysis and Clinical Neurochemistry - https://h001.ssl-redirect.de/www.neurochem.info/
- DZNE – German Center for neurodegenerative Diseases - www.dzne.de/en/about-us/sites/ulm/
- DMSG – German Multiple Sclerosis Society – www.dmsg.de
- KKNMS – Clinical Competence Network for Multiple Sclerosis - https://www.kompetenznetz-multiplesklerose.de/
- DIFUTURE – Data Integration for Future Medicine Project - difuture.de
- EmBioProMS – Multicenter Prospective Study on Serum Biomarkers in Patients with Chronic Progressive Multiple Sclerosis www.msregister.de/forschung/embioproms/
- BioMSeu – Consortium for CSF Biomarker Research - bioms-eu.com
- NEMOS-network – Neuromyelitis Optica Study Group - www.nemos-net.de
- GENERATE – German Network for Research on Autoimmune Encephalitis - en.generate-net.de
- Epiloc – Epiloc study - www.epiloc.de/projekt
Funding
Our research is/was funded by:
- German Center for Neurodegenerative Diseases (DZNE)
- Ministry for Science and Research, Baden-Württemberg
- German Multiple Sclerosis Society (DMSG)
- Federal Ministry of Education and Research (BMBF)
- Chemische Fabrik Karl Bucher
- DMS-Stiftung
- AMSEL-Stiftung
- Bavarian MS foundation (DMSG Bayern)
- University Ulm
- Baustein program University of Ulm
Selected recent publications (last 5 years)
in progress, update soon
Contact
Dr. rer. nat. Steffen Halbgebauer
Zentrum für Biomedizinische Forschung (ZBMF)
Helmholtzstr. 8/1
D-89081 Ulm
