Obesity
Welcome to Obesity Surgery at Ulm University Hospital!
We look forward to welcoming you as a patient to our obesity surgery department at Ulm University Hospital. We have been a certified centre of excellence for obesity and metabolic surgery by the DGAV (German Society for General and Visceral Surgery) since July 2023.
Individual counselling in our Obesity Centre
Our obesity centre offers you an individual consultation tailored to your needs - regardless of whether you are interested in drug treatment or surgery. Your personal situation always takes centre stage. Together with you, we will develop a customised treatment concept that is tailored to your health requirements and goals. If you are looking for sound, empathetic advice, we will be happy to take the time for you.

Obesity is a serious and recognised disease - we accompany you on your way to better health!
Obesity is a serious illness with a variety of causes and health consequences. There is no general answer to the question of which medical centre is the right one to go to in an individual case. At the Obesity Centre at Ulm University Hospital, we therefore provide you with interdisciplinary support - with an experienced team of specialists, structured and personal.
As a rule, the first medical contact is via the family doctor. Based on the body mass index (BMI) and other relevant health data, obesity can be identified and, if necessary, a referral to appropriate specialist services can be arranged - for example to our centre.
At the Obesity Centre at Ulm University Hospital, specialists from various fields work hand in hand:
- Nutritional medicine: for individualised nutritional therapy suitable for everyday use
- Endocrinology / diabetology: to clarify hormonal causes and possible concomitant diseases
- Obesity surgery: for pronounced obesity after conservative measures have been exhausted
- Psychology / behavioural therapy: for support with emotional eating behaviour and sustainable behavioural change
As obesity is considered a chronic disease, our focus is on long-term, holistic therapy. The focus is not on short-term weight reduction, but on improving your overall health prognosis. The basis of every therapy is a detailed diagnosis. We will provide you with comprehensive information about suitable treatment options - such as drug therapies or surgical procedures.
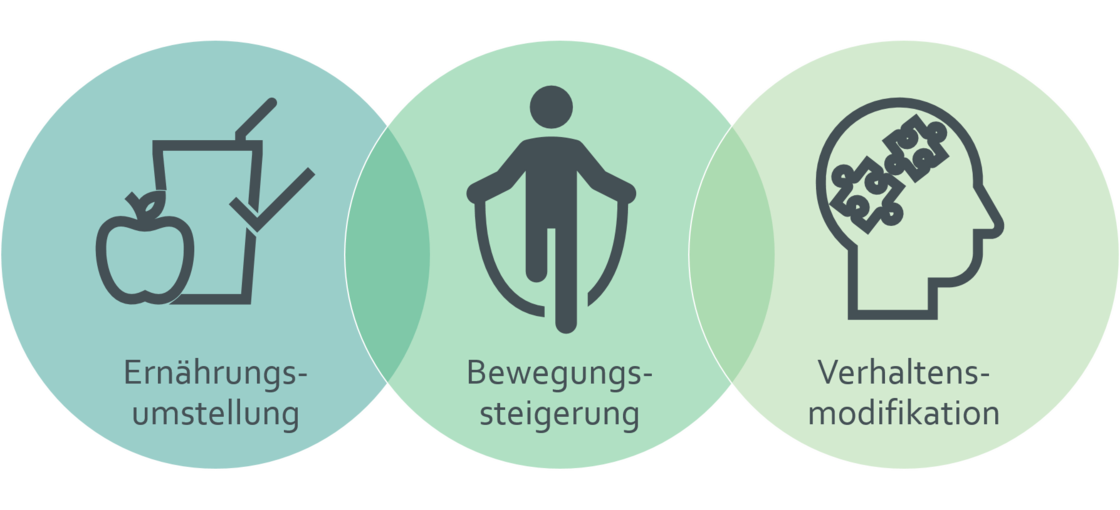
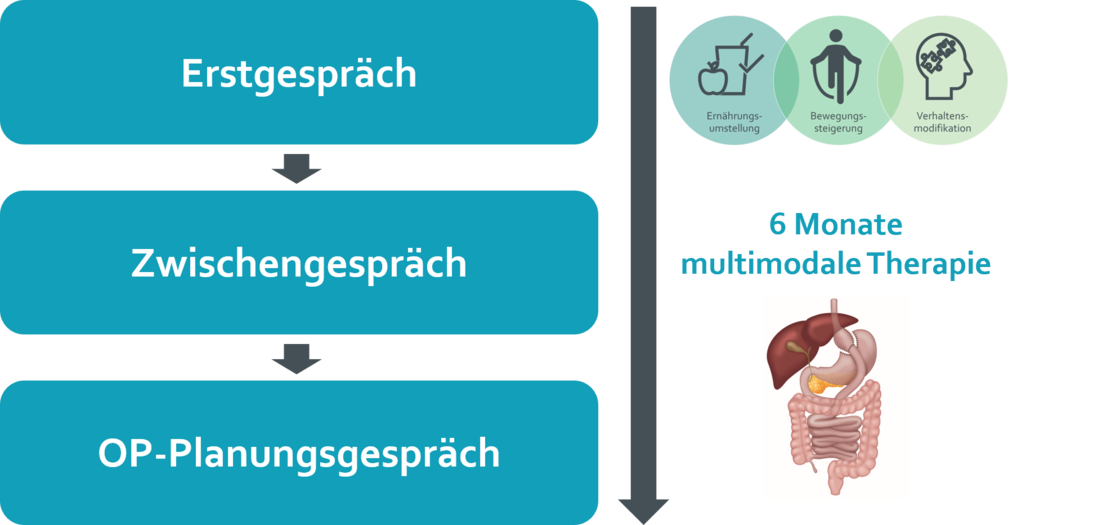
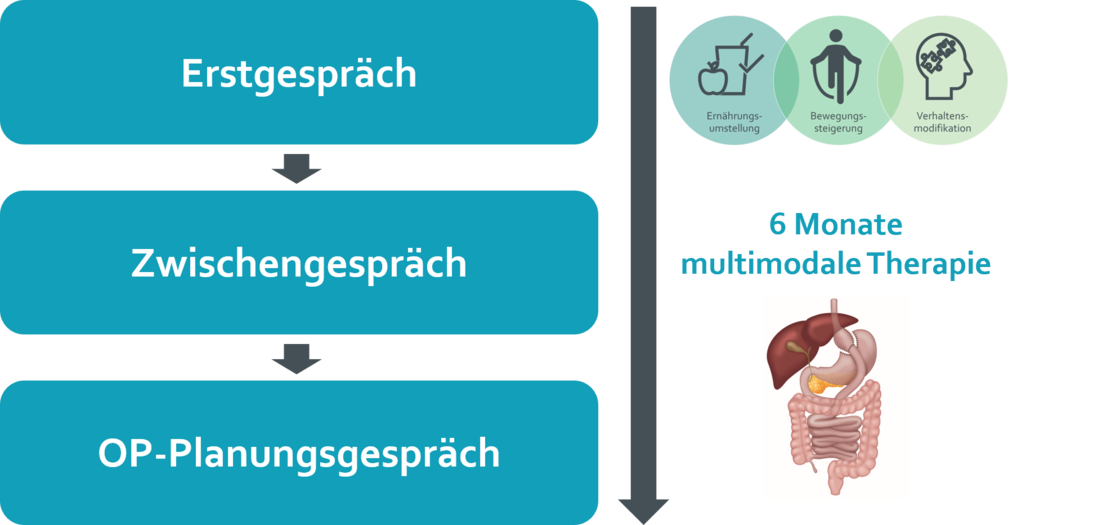
The multimodal concept (MMK)
MMK stands for the multimodal concept for the treatment of morbid obesity. According to the German guideline, obesity should first be treated with a multimodal approach before surgery is planned. The key to success, i.e. sustainable weight reduction, lies in the combination of different therapies, whereby nutrition, exercise and behavioural therapy as well as examinations by specialists such as endocrinologists and ENT specialists play a central role. The multimodal concept usually extends over 6 months. We will be happy to provide you with personalised support in planning and help you to find the right partners for multimodal therapy.
In certain medically justified individual cases, bariatric surgery can also be performed if the multimodal concept (MMK) has not been fully completed. This is possible in particular if conservative treatment is not feasible or the operation appears to be urgently indicated from a prognostic point of view.
Such exceptions are possible in the following constellations in particular:
- A body mass index (BMI) of ≥ 60
- If the BMI is over 50, a shortening of the MMK to three months can be considered in consultation with the treating team
- In the case of severe concomitant or secondary diseases that require rapid surgical intervention and do not allow for a delay
Despite these exceptions, we strongly recommend completing the MMC in full as a rule. It not only serves as medical preparation, but also helps the patient to come to terms mentally with the procedure and the associated changes in everyday life.
We make the decision about your treatment together with you. As your treatment team, we will advise you in detail and make recommendations as to which treatment we believe is medically appropriate.
In addition, a regular professional exchange takes place within the framework of interdisciplinary case conferences. There we discuss individual progressions, review the previous treatment approach and make adjustments if necessary.
However, the final decision is always yours. You decide whether and to what extent you would like to follow the recommended treatment path together with us.
Our consultation hours
| Make an appointment | Monday to Thursday 9:00 am - 3:00 pm Friday 9:00 am - 12:00 pm |
| Consultation hours | Tuesday 8:30 am - 3:00 pm Friday 8:00 am - 1:30 pm |
Outside of these office hours, you can send your request in writing by e-mail to
adipositas@uniklinik-ulm.de. We will deal with your request promptly.
When is surgery an option?
Bariatric surgery can be considered for a body mass index (BMI) over 40kg/m² or a BMI over 35kg/m² with one or more obesity-related secondary or concomitant diseases, such as type II diabetes mellitus, severe fatty liver or blood pressure disease, urinary incontinence or PCO syndrome.
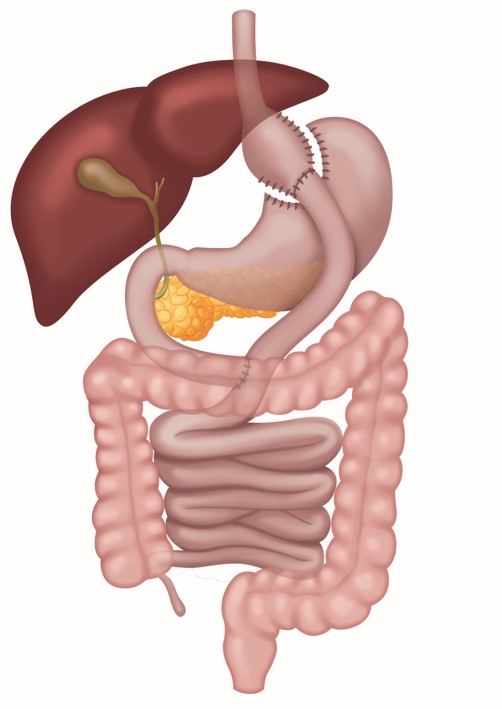
Sleeve gastrectomy
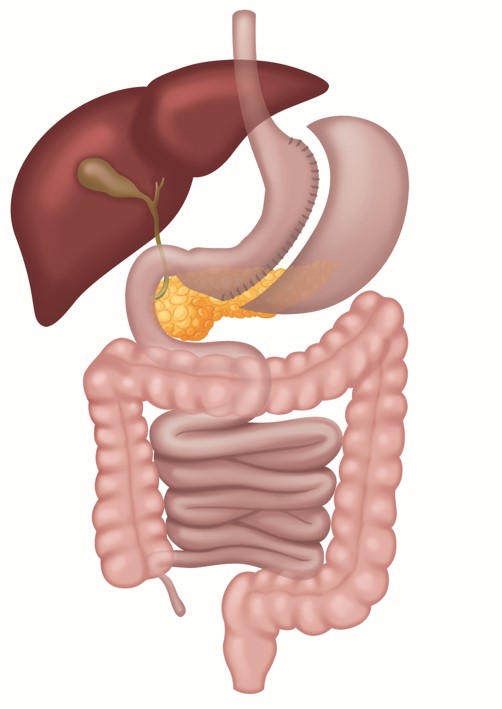
Sleeve gastrectomy - also known as sleeve gastrectomy - is one of the most established procedures in bariatric surgery and is performed most frequently worldwide. A large part of the stomach is permanently removed, leaving only a narrow, tube-shaped residual stomach. The procedure is performed gently using a minimally invasive technique via five small incisions (keyhole procedure).
By reducing the size of the stomach, the food volume is significantly reduced. Even small meals lead to a pronounced feeling of fullness. This is partly due to a change in hormonal signalling, which also contributes to a reduced feeling of hunger.
As part of the stomach is irrevocably removed, this is a non-reversible surgical procedure. However, a subsequent conversion to a gastric bypass may be medically advisable in certain cases.
A possible side effect after gastric sleeve surgery is the increased occurrence of stomach acid, which can flow back into the oesophagus (reflux). Regular endoscopic checks of the oesophagus - approximately every three to five years - are recommended so that any changes to the mucous membrane can be countered at an early stage.
Gastric bypass (ROUX-Y bypass)
The Roux-Y gastric bypass is one of the second most frequently used surgical procedures for obesity worldwide and has proven itself many times over in practice. The procedure is performed using a minimally invasive technique (keyhole surgery) via five small incisions in the skin. The stomach is reduced in size so that only a small stomach pouch remains. The remaining part of the stomach remains in the body, but is no longer involved in the digestive process.
The newly created pouch is then connected to a section of the small intestine further down. The food thus reaches the lower small intestine via a diversion - bypassing the majority of the stomach and duodenum (bypass). A second small intestinal connection is also created so that the food comes into contact with digestive juices such as bile and pancreatic enzymes.
The operation leads to hormonal changes that reduce the feeling of hunger and positively change the metabolism.
changes positively. As a result, less food is consumed. As this also reduces the absorption of important vitamins and trace elements, a lifelong intake of nutritional supplements - especially multivitamin preparations - is necessary. Possible side effects include dumping syndrome and the risk of internal hernias.
Single-anastomosis bypass (OAGB)
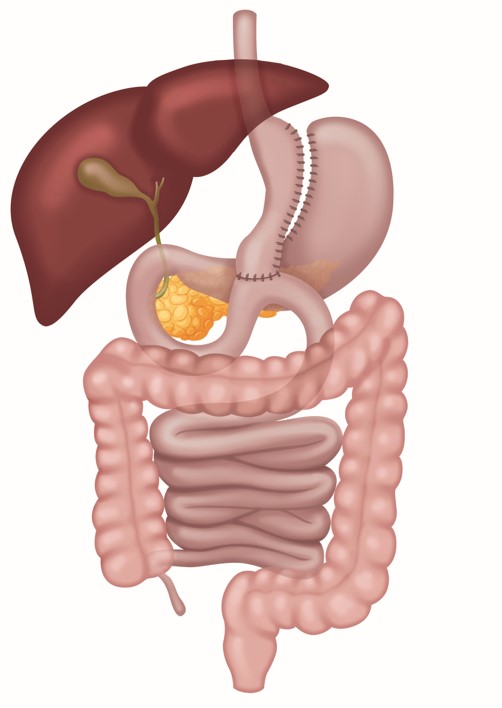
The single anastomosis bypass (also known as one anastomosis gastric bypass (OAGB) or mini gastric bypass) combines a stomach reduction with a bypass procedure (intestinal bypass). An elongated, tubular gastric pouch is formed, similar to a sleeve gastrectomy. In contrast to the classic Roux-Y technique, however, there is only a single connection (anastomosis) between the new small gastric pouch and a lower section of the small intestine.
As only a single connection (anastomosis) is created between the gastric pouch and the small intestine, the duration of the operation is somewhat shorter than with the Roux-Y gastric bypass and the procedure is technically somewhat easier to perform. The single-anastomosis bypass leads to reduced food intake for the same hormonal reasons as the other procedures. A lifelong substitution of a multivitamin preparation is necessary.
One possible consequence of this operation is the reflux of bile into the stomach pouch or even the oesophagus, which can lead to changes in the mucous membrane in the long term.
- S.A.D.I. (Single Anastomosis Duodenoileal Bypass)
- Biliopancreatic diversion
- S.A.S.I. (single anastomosis sleeve ileal bypass)
- Interventions for recurrent (renewed increase in) weight
- Treatment of reflux after sleeve gastrectomy
- Interventions for dumping syndrome
- Complete pouch removal with creation of a connection between the oesophagus and small intestine
We operate WITHOUT a cost commitment!
Prerequisite:
What is important after the operation!
You will notice that the amount of food you eat each day will decrease and that you will have less appetite. Around two years after the operation, your food intake will be roughly comparable to that of a child or senior citizen.
There will be hormonal changes and possibly hair loss, but this will regulate itself again over time. It is therefore advisable to start taking supplements about three months before the operation.
There is a very rapid improvement in diseases such as type 2 diabetes, high blood pressure or lipometabolic disorders. Obese patients can often reduce their medication shortly after the operation, and in some cases even stop taking it altogether.
Regular and lifelong treatment is important for a good and long-term result. We will continue to support you closely with our specialists and are here for you!
Follow-up appointments:
- in the 1st year - check-up appointment 4 weeks after the operation, followed by a check-up appointment every 3 months
- in the 2nd year - a check-up every 6 months
- from the 3rd year - a check-up appointment once a year
Questions & Answers
You have decided to have bariatric surgery and may be wondering what the preparation for the procedure is like and what the first few weeks after the operation will be like.
In this context, we would like to answer some common questions that we are often asked by our patients. Your recovery after surgery will of course depend on various factors, including the surgical procedure you choose. Our recommendations are based on years of experience in bariatric surgery at Ulm University Hospital.
The decision in favour of bariatric surgery is often made after a long process and is not an "easier" route than conservative weight loss attempts. It should be considered if these attempts have failed. Those affected must be aware that this entails considerable changes to their lifestyle.
- In Germany, there is a medical guideline for the surgical treatment of obesity: the AWMF guideline "Surgery for obesity and metabolic diseases".
- For patients with a BMI of 35 to 39, bariatric surgery can be considered if obesity-associated comorbidities (such as type 2 diabetes, heart failure, sleep apnoea, etc.) are present and conservative therapy has been exhausted.
- With a BMI of 40 or more, bariatric surgery is possible if there are no concomitant diseases or contraindications and conservative therapy has also been exhausted, provided that comprehensive information is provided.
MMK stands for the multimodal concept for the treatment of morbid obesity. According to the German guideline, obesity patients should first undergo multimodal treatment before surgery is planned. This includes nutrition, exercise and behavioural therapy as well as examinations by specialists such as endocrinologists and ENT specialists.
We will be happy to provide you with personalised support in planning and help you find the right partners for multimodal therapy.
The multimodal concept usually extends over 6 months.
The key to success, i.e. sustainable weight loss, lies in the combination of different therapies, with nutrition, exercise and behavioural therapy playing a central role. We are happy to provide you with personalised support to help you plan and find the right partners for implementing multimodal therapy.
If you are unable to carry out an exercise programme due to your illness, try physiotherapy or rehabilitation sports. There you will receive professional support and an individually adapted programme.
If this is not possible either, you will need a statement from an orthopaedic specialist explaining the reasons for this.
Not everyone feels comfortable talking in a self-help group, and that is completely understandable. However, self-help forums offer an excellent opportunity to get in touch with other sufferers anonymously.
After your presentation at our bariatric centre, you will begin the multimodal concept, which lasts at least six months. If you fulfil the conditions for bariatric surgery, you can have the operation performed without a prior health insurance check. After the operation, we will bill your health insurance company for the operation, as with any other inpatient treatment.
Depending on their state of health, our patients stay in hospital for around 2 to 3 days.
In the first 24 hours after the operation, pain may occur in the shoulder and chest region due to the gas used. The wounds may also be uncomfortable at first. Effective pain medication is available to help you get back on your feet quickly. The need for pain medication is individual and you can contact us at any time if you are in pain. Many patients report that the abdominal wall feels like sore muscles or a muscle cramp after the operation. If you experience severe pain, you should inform us or, if you are already at home, visit the emergency department.
- Mild nausea may occur more frequently at the beginning. Medication is available for this, which your GP can prescribe. If the nausea occurs several times, you should contact the clinic where you had the operation again.
- If you suspect that one of your wounds is infected, please contact your GP or our clinic immediately. Early treatment can help to avoid more serious problems.
The return to work depends heavily on the physical strain. It is advisable to discuss this with your surgeon. After laparoscopic surgery, you should refrain from lifting weights over 5 kg for about 4-5 weeks. In the case of open surgery, this period should be at least 6 weeks.
As a rule, you can walk for up to 30 minutes after about a week. You should then gradually increase your activity. After 4 to 6 weeks, all types of sport are possible. If you experience discomfort during exercise or have existing pain, it is advisable to reduce the intensity of the exertion.
We strongly recommend that you wait around 1.5 to 2 years after the operation before becoming pregnant in order to minimise the risks for you and your unborn child. However, if an unwanted pregnancy occurs immediately after the operation, we recommend that you visit our centre regularly.