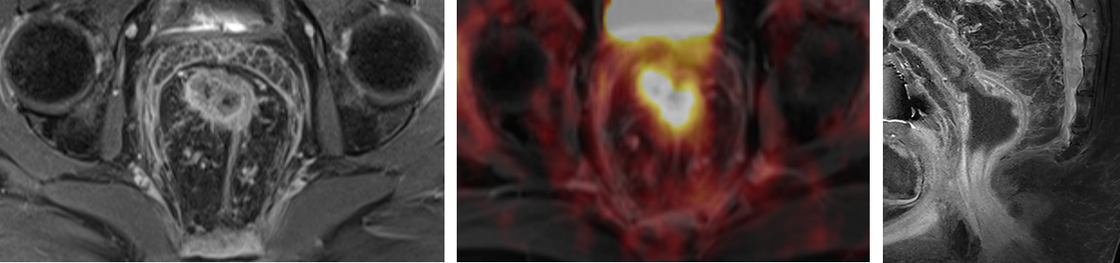
FDG-PET/MRI in rectal cancer
In recent years, an increasing number of therapy options for rectal cancer have emerged, ranging from primary surgery to intensified neoadjuvant therapy concepts, usually consisting of a combination of radiation and chemotherapy, to non-surgical therapy strategies (so-called "watch and wait" concept). Due to the multitude of options, however, it is becoming increasingly difficult for the treating physicians to select the optimal therapy option in the individual case on the basis of the usual findings.
It is possible that the combination of MRI together with the metabolic information from FDG-PET can provide helpful additional information. Therefore, we are currently investigating the value of PET/MRI in the initial diagnosis and primary therapy decision as well as in the re-evaluation after neoadjuvant therapy, especially in the decision for surgery or non-operative management ("watch and wait").
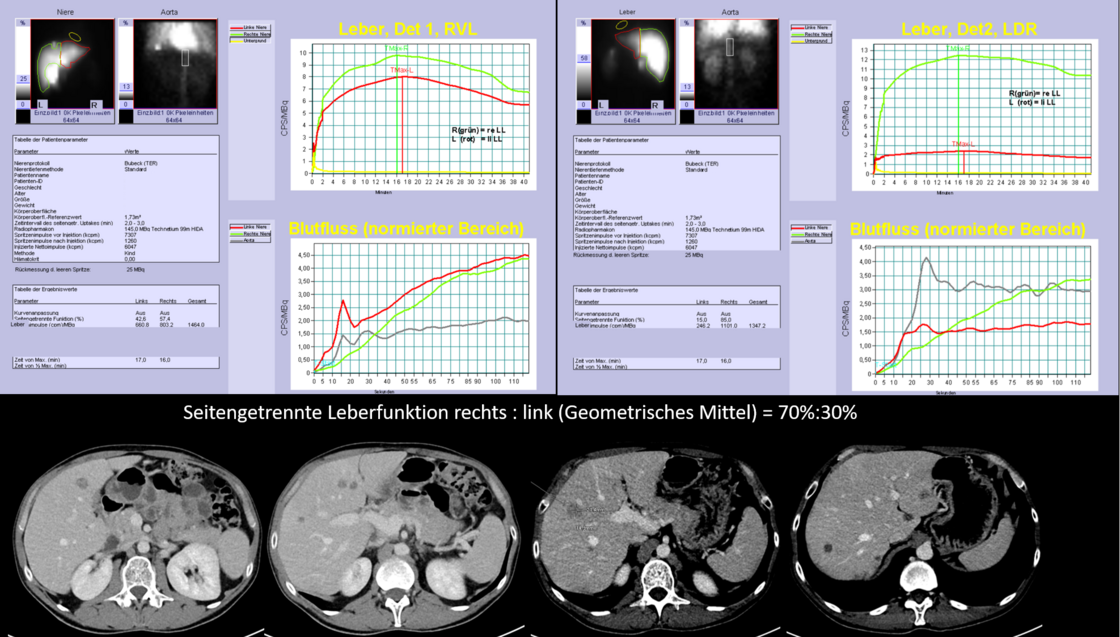
Liver volumetry and liver function scintigraphy
After extensive liver resections (so-called major resections), postoperative liver failure is the main cause of postoperative mortality. The occurrence of postoperative liver failure depends on the extent of resection and the functional liver capacity, which may be limited by pre-existing liver diseases (e.g. cirrhosis, fatty liver, etc.) or by previous chemotherapy.
The combination of preoperative volumetry with precise measurement of the remaining liver tissue together with liver function scintigraphy (e.g. Tc-99m-HIDA or Tc-99m-Mebrofenin) to investigate the functional capacity of the remaining liver tissue, can provide helpful information to prevent postoperative liver failure. Therefore, the combination of these two examinations is offered in the surgical planning of complex liver interventions (e.g. two-stage liver resections in the so-called ALPPS procedure) and the effect of this advanced surgical planning is investigated.
Intraoperative resection planning in liver surgery (IOUS, ICG, 3D reconstruction)
In minimally invasive or robotic resection of liver tumours, intraoperative resection planning is crucial as the surgeon lacks palpatory or manual control. In order to correctly assess the positional relationship between the tumour and the relevant blood vessels and bile ducts, a combination of intraoperative ultrasound directly on the liver surface together with fluorescence imaging using indocyanine green (ICG) and 3D reconstructions of the preoperative imaging is therefore used. In this way, it is usually possible to completely remove the tumours while preserving the relevant blood vessels and bile ducts.
