Overview
Dear Patient,
a benign thyroid disease can be treated in several ways. First of all, there is the possibility to take medication, furthermore surgery and radioiodine therapy are available.
Medication for hyperthyroidism can cause severe side effects and lead to further growth of the thyroid gland. Often, even after starting drug treatment, if the disease persists, definitive therapy, either surgery or radioiodine therapy, must be performed. The success of these two methods seems to be largely equivalent.
Mandatory for surgery, the patient receives anesthesia because during the procedure the patient must lie absolutely still and special attention must be paid to the vocal cord nerves. Injury could possibly lead to permanent paralysis of one or both vocal cords. Swelling and pain may occur after surgery and a scar will remain.
The side effects of radioiodine therapy are considered to be much less. This is a treatment that has been established for more than 40 years and is extremely effective. A radioactive form of iodine, iodine-131 has a radiation that reaches only a few millimeters in the tissue. It elegantly and selectively treats only those areas of the thyroid gland that cause the actual hyperfunction, while sparing other healthy tissue. Even the smallest areas can be treated that appear inconspicuous in ultrasound, but nevertheless contain cells that then cause the defective hyperfunction independently of regulatory mechanisms.
A small amount of radiation from iodine-131 escapes from the body and is used to check the effect of the therapy. It is also the reason why in Germany radioiodine therapy may only be performed during a minimum 48-hour inpatient stay.
Radioiodine therapy
The iodine-131 is administered in the form of a small capsule, and reaches the hyperactive areas of the thyroid gland via the bloodstream, irradiating them precisely. The iodine that is not absorbed into the thyroid gland is excreted in the urine within the next few hours. In most cases, a single therapy is sufficient to achieve the full effect; rarely is a second one required. Sometimes after therapy, as after surgery, it may be necessary to take thyroid hormone tablets. They are used to prevent further growth in size. Rarely, a sore throat, similar to a cold, may occur after therapy. If this occurs, the throat can be cooled and by taking anti-inflammatory substances, the patient obtains relief and freedom from symptoms after a short time. Unfortunately, for reasons of radiation protection, visitors are not allowed during the inpatient stay. However, a short walk in the ward corridor or in the fresh air in the small patient garden is of course possible at any time. The bright and spacious single rooms of the ward are equipped with windows, free TV and radio as well as a bathroom. Special structural features of these rooms are specially shielded walls and windows as well as a so-called decay system for collecting waste water. The length of stay depends on the type of disease, the dose and the individual excretion and is usually between 2 and 5 days. After discharge, depending on the patient, we recommend keeping a few more days away from small children and pregnant women, after which no further precautions are necessary.
Would you like to get more information or make an appointment for treatment? We will be happy to advise you!
(see contact above)
Other types of therapy
PRRT
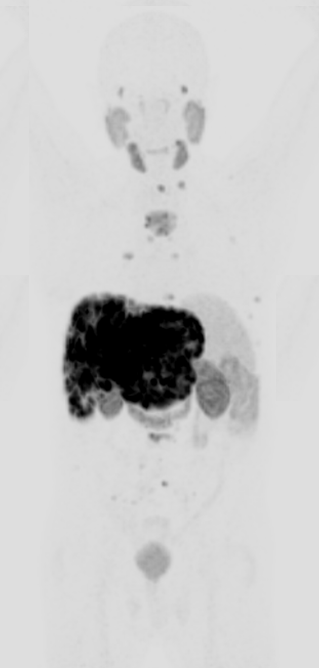
Neuroendocrine tumor cells have special receptors on their surface that serve as "docking sites" for the hormone somatostatin. These so-called somatostatin receptors also occur naturally in other body tissues, but their density is particularly high on the cells of certain neuroendocrine tumors.
Nuclear medicine uses a special substance (DOTAiTATE) that can bind to the somatostatin receptors. The substance is coupled with radioactive elements in the laboratory and can be introduced into the body in the form of an injection or infusion. In this way, the radioactive molecules enter those cells that have somatostatin receptors. Depending on the type of radioactive labeling, precise, sensitive diagnostics (DOTAiTATE - PET/CT) or systemic treatment (radiopeptide therapy, PRRT) are thus possible.
For therapy, DOTAiTATE is chemically combined with radioactive lutetium-177 (177Lu). The substance labeled in this way accumulates in the body exactly as it was detected in advance on the PET/CT images and is retained in the respective cells for a longer period of time. The lutetium emits high-energy beta rays that have a short range of only a few millimeters in the body, but transfer high energy doses to the diseased tissues along the way. In this way, a precise, targeted "internal irradiation" of these tissues takes place.
In this way, metastasized neuroendocrine tumors can be treated in a targeted manner. In many cases, the tumor mass can be reduced, the course of the disease can be slowed down, and any existing neuroendocrine symptoms can be improved. The therapy has been used in many places for many years and is generally well tolerated with few side effects.
The indication for treatment of a neuroendocrine tumor is typically made on an interdisciplinary basis by internal medicine-oncology, endocrinology, surgery, and nuclear medicine. The actual treatment then takes place in the nuclear medicine therapy ward and is associated with a stay of about three days. The therapy substance is applied on the first day of the stay in the form of an intravenous infusion, with other drugs usually also being administered to improve tolerance. For certain indications in certain neuroendocrine tumours, we have also been offering the approved therapeutic Lutathera® (lutetium-177-oxodotreotide) for therapy since mid-2022.
The treatment consists of several therapy cycles, which are carried out at intervals of several months. Depending on response and tolerability, two to four or even more such cycles may be administered.
Would you like more information or to make an appointment for treatment? We will be happy to advise you!
(see contact above)
PSMA - Therapy
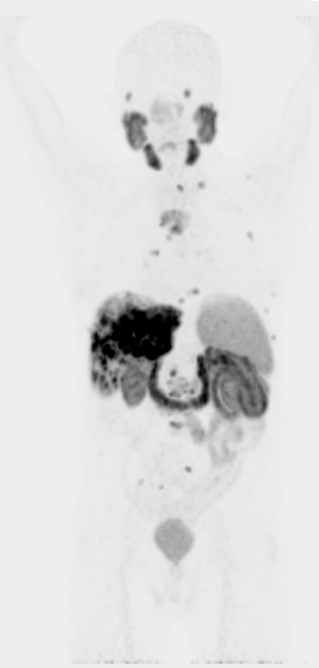
Radionuclide therapy with lutetium-177-PSMA (in short "PSMA therapy") is a modern, innovative therapy method that is becoming increasingly widespread in the treatment of certain stages of metastatic prostate carcinoma. The therapy is usually very well tolerated and provides promising initial results.
Prostate-specific membrane antigen (PSMA) occurs naturally in many body tissues, but is found in particularly high levels on prostate cancer cells. This makes it suitable as a target structure for the diagnosis and therapy of prostate carcinoma and its metastases.
In nuclear medicine, special substances are used that can bind to the PSMA. These so-called ligands are coupled with radioactive substances in the laboratory and introduced into the body in the form of an injection. In this way, the radioactive molecules enter those cells that carry the PSMA. Depending on the type of radioactive labeling, precise, sensitive diagnostics (PET/CT) or treatment (PSMA therapy) are thus possible.
Therapy involves chemically combining the ligands with radioactive lutetium-177 (177Lu). The substance accumulates in the body exactly as it was detected in advance on the PET/CT images and is retained in the respective cells for a longer period of time. The lutetium emits high-energy beta rays that have a short range of only a few millimeters in the body, but transfer high energy doses to the diseased tissues along the way. In this way, a precise, targeted "internal irradiation" of these tissues takes place.
The decision as to when in the course of treatment PSMA therapy is appropriate is typically made on an interdisciplinary basis by oncologists, urologists and nuclear medicine specialists. The actual treatment takes place on the nuclear medicine therapy ward and usually involves a three-day inpatient stay. Since 05/2023, it has also been possible to use the approved therapeutic Pluvicto® (lutetium-177 vipivotide tetraxetan), which, according to studies, can also be indicated and used earlier in the therapy cascade.
Would you like more information or to make an appointment for treatment? We will be happy to advise you!
(see contact above)
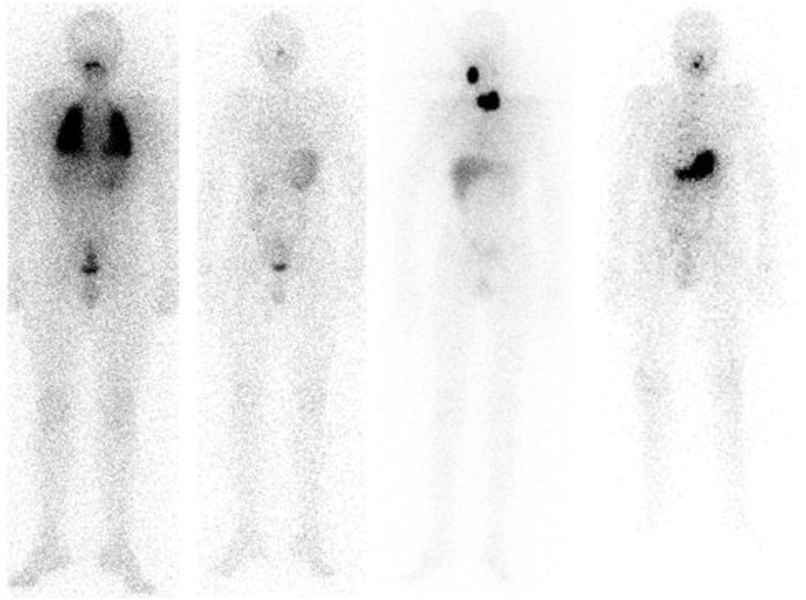
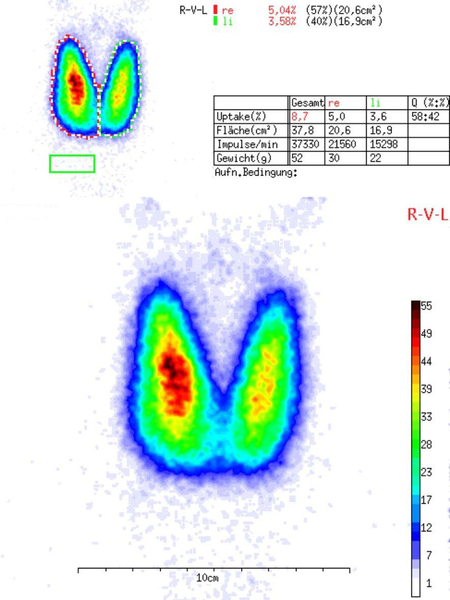
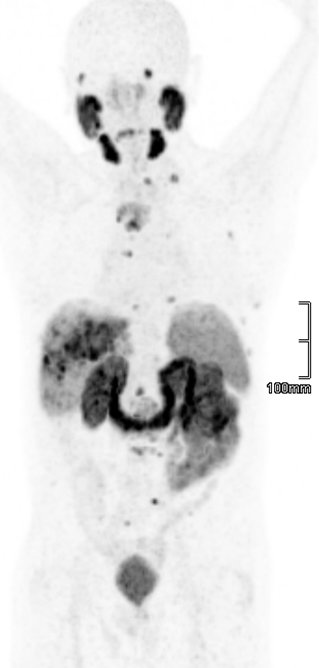
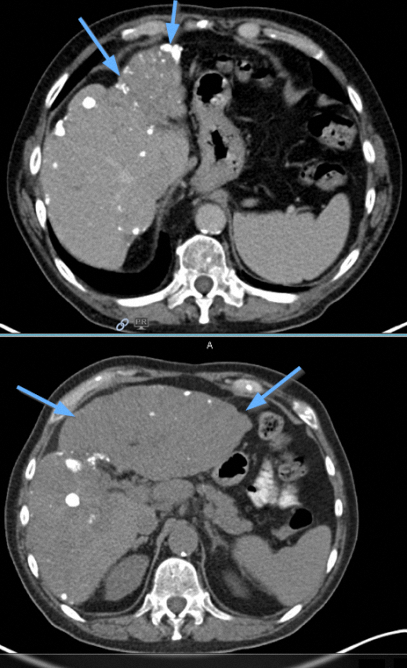
Case study PSMA therapy
mCRPC (73 J), GS: 3+4 =7; ED 02/2007.
Histology from liver metastases: Metastasis from a poorly differentiated, partially neuroendocrine dedifferentiated prostate adeno-ca., G3.
Condition after ADT including Abiraterone, 9x Docetaxel, 28x Cabazitaxel
PSMA PET/CT

SIRT
Selective internal radiotherapy (SIRT) is a minimally invasive therapy for the treatment of tumor tissue in the liver (primary liver tumors and possibly also liver metastases from other diseases).
During the treatment, small radioactively loaded beads (called microspheres) are introduced into the liver. These microspheres become trapped in the smallest blood vessels in the well perfused tumor tissue. The radioactive substance yttrium-90 contained in the spheres emits therapeutically effective beta radiation over several days. The radiation transmits high local energy doses, although its range in the body is only about one centimeter.
Thus, a high radiation effect is achieved in the tumor tissue while sparing the surrounding healthy portions of the liver. The tumor tissue is substantially damaged in this way, preventing further growth and spread. The tumor foci can thus be reduced in size or, under certain circumstances, completely removed.
SIRT exploits a special feature of the liver's blood vessel supply. While healthy liver tissue receives its blood supply mainly from the hepatic vein (portal vein), tumor tissue is usually supplied with blood mainly from the hepatic artery. The microspheres are therefore introduced into the hepatic artery via the groin using a special catheter (angiography) in collaboration with physicians from the Department of Radiology.
The treatment can halt further progression of the disease for some time and preserve the quality of life as long and as well as possible.
The decision as to whether SIRT can be usefully applied is typically made within the framework of an interdisciplinary tumor conference with colleagues from all medical disciplines involved.
The necessary preliminary examinations and the actual treatment are carried out in cooperation with physicians from the clinics of nuclear medicine and radiology (combined in the Center for Imaging), as well as in cooperation with the Internal Medicine I. In order to reduce side effects or complications, the entire liver is not usually treated at the same time, but rather parts of the liver are treated step by step in two therapy cycles several weeks apart. The individual treatment cycles each take place during a stay of about three days on an internal medicine ward.
Would you like more information or to make an appointment for treatment? We will be happy to advise you!
(see contact above)
Xofigo - Therapy
Treatment with radium-223 (Xofigo®) is suitable for patients with painful bone metastases from a prostate carcinoma that no longer responds to hormonal treatment (so-called castration-resistant stage), when there are no known distant metastases in other organs.
Where there are metastases in the skeletal system, there is typically a marked increase in bone metabolism. Radium accumulates in the bones in a manner similar to dietary calcium, and depending on bone metabolism, to a particularly high degree where bone metastases are located. The radium emits a high-energy alpha radiation, which, however, has only a very short range in the body. In this way, a targeted internal irradiation of the bone metastases succeeds, while surrounding, non-diseased body tissues are largely spared. Thus, the improvement of a pain symptomatology and a prolongation of the survival time can be achieved.
The decision as to whether therapy with Xofigo® is appropriate is typically made on an interdisciplinary basis by urologists, oncologists and nuclear medicine specialists. Since the therapeutically effective radiation does not leave the body, treatment is possible on an outpatient basis. It is offered and performed in the Department of Nuclear Medicine.
Typically, patients receive six injections of Xofigo® at one-month intervals. If necessary, the intervals between injections can also be extended. Likewise, in individual cases, more or less than six injections of Xofigo® may be administered.
Would you like more information or to make an appointment for treatment? We will be happy to advise you!
(see contact above)